CMS has released the Quality Payment Program (QPP) Final Score & Performance Feedback Reports for the 2022 Performance Year, along with the MIPS Payment Adjustments for Payment Year 2024. Understanding your feedback reports, and using them to identify areas of improvement is key to optimizing your performance in this program year to year.
Our Kentucky REC expert advisors will guide you through the Feedback Report and explain how you can use this information to help you finish 2023 successfully and strategize for a strong start in 2024!
We will discuss how to navigate your feedback reports, help you understand payment adjustments, and provide you with insights to aid in identifying your opportunities and strengths across the four performance categories. We’ll also share how you can leverage that information to help you plan for continued success with this program in the future.
QPP Year 7: Interpreting QPP Feedback Reports*
Tuesday Oct 10, 2023 @ 12PM ET
*This webinar is for Kentucky REC contracted QPP clients only. If you are interested in this topic and would like to learn more about becoming a client, please contact us at (859) 323-3090 or email us at KYRec@uky.edu. We aim to be your trusted healthcare advisor!


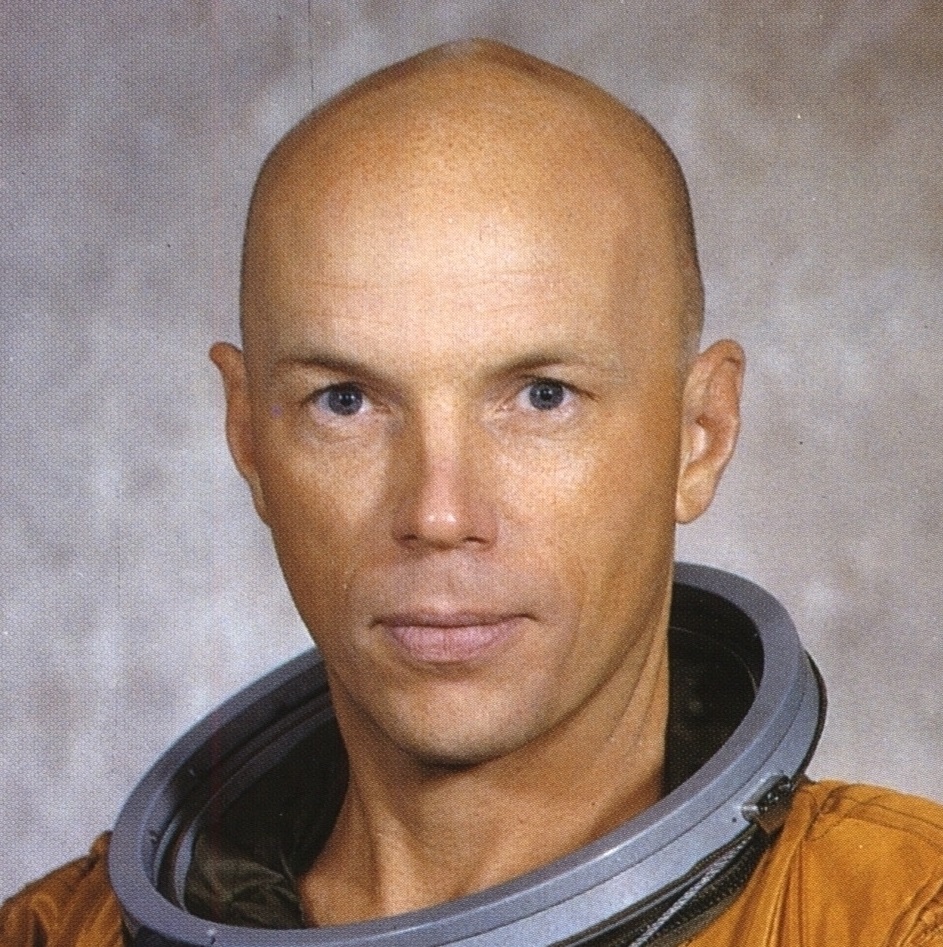 KEYNOTE SPEAKER: STORY MUSGRAVE
KEYNOTE SPEAKER: STORY MUSGRAVE
 Kentucky REC expert advisors are hosting a webinar on the Medicare Promoting Interoperability (PI) Program for Eligible Hospitals and Critical Access Hospitals. We will review the 2023 Medicare PI requirements and highlight the recently released FY 2024 Inpatient Prospective Payment System (IPPS) proposed rule.
Kentucky REC expert advisors are hosting a webinar on the Medicare Promoting Interoperability (PI) Program for Eligible Hospitals and Critical Access Hospitals. We will review the 2023 Medicare PI requirements and highlight the recently released FY 2024 Inpatient Prospective Payment System (IPPS) proposed rule.


